Bariatric surgery consists of surgical procedures performed on the stomach or intestines to induce weight loss. In this realm, the SADI procedure stands out as a groundbreaking approach in the battle against obesity. SADI stands for “Single Anastomosis Duodenal Ileostomy,” and it offers a promising solution for individuals struggling with severe obesity and related health complications.
This inclusive overview aims to shed light on the intricacies of the SADI surgery procedure, exploring its benefits, risks, and potential outcomes.
What is SADI Surgery?
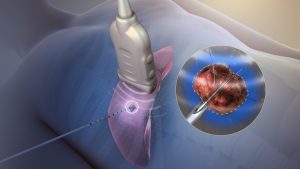
SADI surgery combines elements of two well-established bariatric procedures: sleeve gastrectomy and duodenal switch. During the procedure, a significant portion of the stomach is removed to reduce its size, limiting food intake. Additionally, the surgeon reroutes a portion of the small intestine to decrease the absorption of calories and nutrients. The combination of these two measures delivers the patient’s desired weight loss.
How Does SADI Surgery Work?
The first step in the SADI procedure involves the removal of 70-80% of the stomach, leaving behind a narrow sleeve-shaped pouch. This cuts down the amount of food that can be eaten at one time. Following sleeve gastrectomy, the surgeon reroutes the small intestine to limit the absorption of calories and nutrients while maintaining the natural flow of digestive juices.
Benefits of SADI Surgery
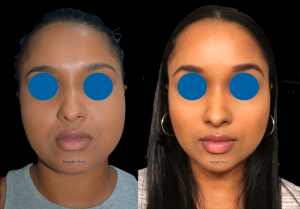
The primary benefit of SADI surgery is the resulting substantial and sustained weight loss, making it an effective option for individuals with severe obesity. Additionally, SADI surgery can lead to improvements in obesity-related debilities such as diabetes, hypertension, and sleep apnea. Because SADI surgery preserves a portion of the small intestine, it reduces the risk of problems with absorbing nutrients from food. Studies indicate that SADI surgery may offer better long-term weight loss outcomes than other bariatric procedures.
Things to Consider Before Trying SADI
While SADI surgery is generally very safe, there are some risks that should be considered. These include nutritional deficiencies, which may occur due to the decreased absorption of nutrients. Long-term vitamin and mineral supplements may be required in some cases. Another concern is “Dumping Syndrome,” in which some individuals may experience nausea, vomiting, and diarrhea, particularly after consuming high-sugar or high-fat foods. There is also the remote possibility of complications such as bowel obstruction, ulceration, and intestinal leakage, though these are rare.
Is SADI Surgery Right for You?
The decision to undergo SADI surgery should be made in consultation with a qualified bariatric surgeon. Candidates for SADI surgery typically have a body mass index (BMI) of 40 or higher, or a BMI of 35 or higher with obesity-related health conditions. Importantly, SADI should be paired with substantial lifestyle changes, including changes to diet and a regular exercise program.
Summing Up SADI Surgery
This procedure offers a promising new approach to weight loss and obesity-related health. Overall, the potential benefits of SADI surgery outweigh the risks, making it a worthwhile option for those who struggle with severe obesity. By understanding the intricacies of the SADI procedure and working closely with healthcare providers, patients can make informed decisions about their weight loss journey and wellness goals.